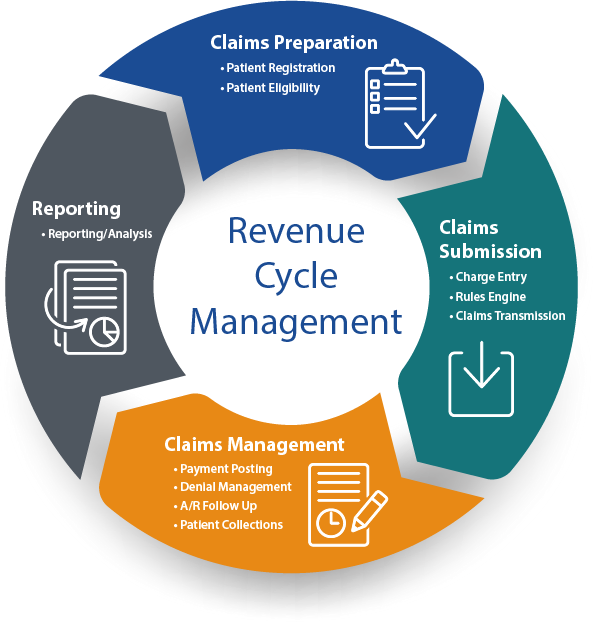
Revenue Cycle management
Revenue Cycle Management (RCM) in medical billing refers to the process of effectively managing the financial aspects of a healthcare practice’s operations, from the initial patient appointment or encounter to the final reimbursement received for services provided. The primary goal of revenue cycle management is to optimize the revenue generation of healthcare providers by ensuring accurate and timely billing, claim submission, reimbursement, and payment collection. This involves a series of interconnected steps that collectively aim to maximize revenue while minimizing delays and inefficiencies. Here are the key components of revenue cycle management in medical billing:
Our Team Will be Incharge of
Patient Registration and Scheduling
The process starts with capturing accurate patient demographic and insurance information during registration and scheduling appointments.
Eligibility Verification
Before providing services, the provider verifies the patient’s insurance coverage to determine their eligibility and benefits, which helps avoid billing issues later.
Point of Care Documentation
Accurate and comprehensive documentation of patient care details, including diagnoses, treatments, procedures, and medications.
Coding
Medical coders assign appropriate codes (CPT, ICD-10, HCPCS) to the services provided during the patient encounter. Accurate coding is crucial for correct billing.
Claim Creation
Based on the documented services and coded information, claims are generated with all necessary details for submission.
Claim Submission
Claims are electronically submitted to insurance companies or payers. This step involves ensuring accurate and complete information to expedite processing.
Claims Adjudication
Insurance companies review and process claims. This includes assessing claims for accuracy, determining reimbursement rates, and either accepting or denying claims.
Reimbursement and Payment
Upon claim approval, insurance companies send reimbursement to the healthcare provider. Patients may also make payments for any outstanding balances.
Denial Management
If a claim is denied, it requires investigation, correction, and resubmission. Effective denial management helps prevent revenue loss.
Appeals
In case of claim denials or underpayments, healthcare providers can appeal with additional documentation to seek proper reimbursement.
Patient Billing and Collections
Patients are billed for any remaining balance after insurance reimbursement. The practice handles collections, payment plans, or other arrangements.
Payment Posting
Payments received from insurance companies and patients are accurately posted to patient accounts, reflecting the financial transactions.
Financial Reporting and Analysis
Comprehensive reports are generated to provide insights into the financial health of the practice, including revenue trends, reimbursement rates, and outstanding balances.
Effective revenue cycle management ensures that healthcare providers receive the appropriate reimbursement for the services they provide, leading to financial stability, efficient operations, and the ability to continue delivering quality patient care.