Practice Management
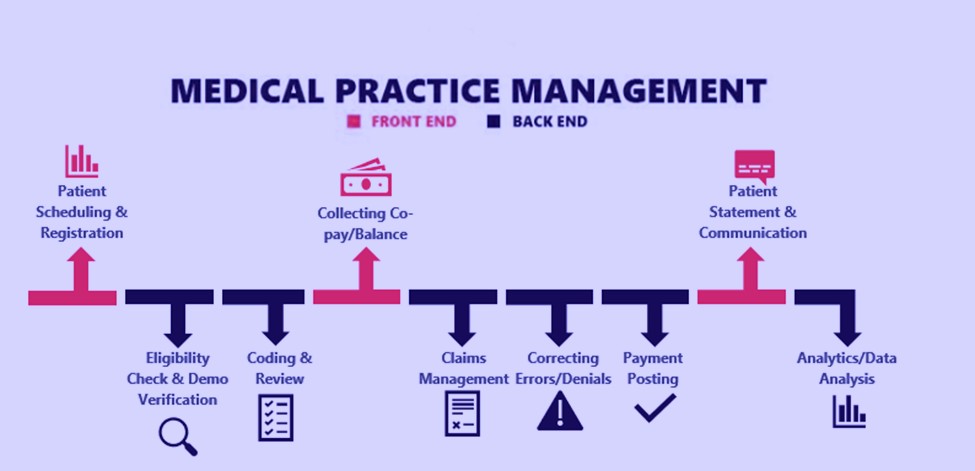
Practice management in medical billing refers to the comprehensive process of overseeing and coordinating the administrative and operational aspects of a medical practice or healthcare facility. It involves various tasks related to the efficient functioning of the practice, including patient scheduling, billing, coding, insurance claims processing, electronic health records (EHR) management, and more. The primary goal of practice management in medical billing is to ensure that the practice operates smoothly, patients are provided with quality care, and financial aspects are effectively managed.
Key components of practice management in medical billing include:
Patient Scheduling
The process starts with capturing accurate patient demographic and insurance information during registration and scheduling appointments.
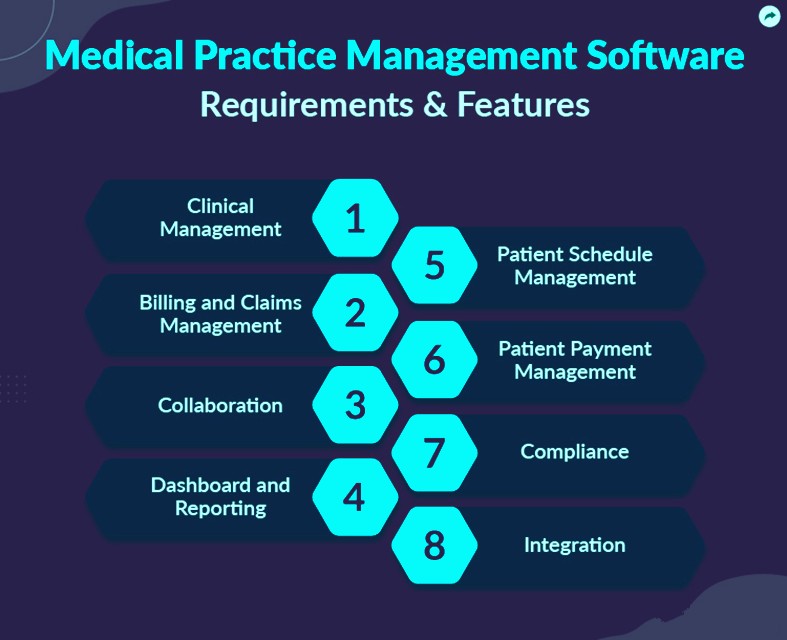
Billing and Coding
Before providing services, the provider verifies the patient’s insurance coverage to determine their eligibility and benefits, which helps avoid billing issues later.
Insurance Claims Processing
Accurate and comprehensive documentation of patient care details, including diagnoses, treatments, procedures, and medications.
Revenue Cycle Management
Medical coders assign appropriate codes (CPT, ICD-10, HCPCS) to the services provided during the patient encounter. Accurate coding is crucial for correct billing.
Electronic Health Records (EHR) Management
Based on the documented services and coded information, claims are generated with all necessary details for submission.
Patient Communication
Claims are electronically submitted to insurance companies or payers. This step involves ensuring accurate and complete information to expedite processing.
Staff Management
Insurance companies review and process claims. This includes assessing claims for accuracy, determining reimbursement rates, and either accepting or denying claims.
Compliance
Upon claim approval, insurance companies send reimbursement to the healthcare provider. Patients may also make payments for any outstanding balances.
Financial Reporting
If a claim is denied, it requires investigation, correction, and resubmission. Effective denial management helps prevent revenue loss.
Technology Integration
In case of claim denials or underpayments, healthcare providers can appeal with additional documentation to seek proper reimbursement.
Effective practice management in medical billing is crucial for maintaining a profitable and well-functioning healthcare practice. It requires a combination of organizational skills, attention to detail, knowledge of medical billing and coding, understanding of insurance processes, and familiarity with healthcare regulations. Many healthcare practices also hire dedicated practice managers or outsource practice management services to specialized companies to ensure the smooth operation of their administrative tasks.
Medical Practice Management Flow